Home Sleep Apnea Test 2026: Complete Guide to At-Home Sleep Studies
Learn how to diagnose sleep apnea from the comfort of your own bed with HSAT devices like NightOwl and WatchPAT. Discover accuracy rates, costs, insurance coverage, and what to do after getting your results.
The home sleep apnea test (HSAT) has revolutionized how we diagnose obstructive sleep apnea, allowing millions of patients to skip the sleep laboratory and get tested in their own beds. According to the Sleep Foundation, According to the American Academy of Sleep Medicine, home sleep tests now account for over 70% of all sleep apnea diagnoses in uncomplicated cases, offering a convenient, cost-effective alternative to in-lab polysomnography that delivers results you can trust. When combined with innovative treatments like the Back2Sleep intranasal orthosis, you can move from diagnosis to relief in record time.

Whether you're experiencing loud snoring, waking up gasping for air, or feeling exhausted despite getting eight hours of sleep, an at-home sleep study can provide the answers you need. This comprehensive guide covers everything from choosing the right device to interpreting your results and finding the best treatment options. Learn more about sleep apnea diagnostic testing from Mayo Clinic.
Home Sleep Testing Statistics for 2026
Key Insight: Studies published in the Journal of Clinical Sleep Medicine show that home sleep tests correctly identify moderate-to-severe sleep apnea in approximately 85% of cases when used in appropriate patient populations.
What is a Home Sleep Apnea Test (HSAT)?
A home sleep apnea test, also known as a home sleep test (HST) or out-of-center sleep testing (OCST), is a portable diagnostic device that measures your breathing patterns, blood oxygen levels, and heart rate while you sleep in your own bed. Unlike in-lab polysomnography, HSAT focuses specifically on detecting obstructive sleep apnea (OSA) rather than a full range of sleep disorders.
What Does a Home Sleep Test Measure?
Airflow Detection
Nasal cannula or thermistor sensors measure breathing patterns, detecting complete cessations (apneas) and partial reductions (hypopneas) in airflow throughout the night.
Oxygen Saturation (SpO2)
Pulse oximetry continuously monitors blood oxygen levels via a finger sensor, identifying dangerous desaturations that occur during breathing interruptions.
Heart Rate Variability
Photoplethysmography tracks cardiac rhythm changes that accompany apnea events, providing insight into cardiovascular stress during sleep.
Body Position & Movement
Accelerometers detect sleeping position and movement, helping identify positional sleep apnea where events occur primarily when lying on your back.
Why Choose an At-Home Sleep Study?
The advantages of home sleep testing extend beyond mere convenience. Research from Stanford Sleep Medicine demonstrates that patients tested at home experience less "first-night effect" - the phenomenon where unfamiliar environments alter sleep patterns. This means your results better reflect your actual sleeping habits.
Natural Sleep Environment - Test in your own bed with your own pillow, producing results that accurately represent your typical sleep.
Significantly Lower Cost - HSAT typically costs $150-$500 compared to $1,500-$3,500 for in-lab studies, with most insurance covering both options.
No Waiting Lists - Skip the 4-8 week wait times common at sleep centers and get tested within days of receiving your device.
Faster Results - Many services provide preliminary results within 2-3 business days, accelerating your path to treatment.
Best Home Sleep Apnea Test Devices 2026
The home sleep test market has evolved dramatically, with 2025 bringing several innovative devices to consumers. Here's how the leading options compare:
| Device | Type | Channels | Accuracy | Cost Range | Best For |
|---|---|---|---|---|---|
| ResMed NightOwl | Fingertip sensor | 3 (PAT, SpO2, actigraphy) | 85-90% | $189-$299 | Simplicity, minimal setup |
| WatchPAT ONE | Wrist-worn + finger | 7 (including sleep staging) | 89-91% | $250-$400 | Comprehensive data, sleep staging |
| Alice NightOne | Traditional HSAT | 4 (airflow, effort, SpO2, position) | 82-87% | $200-$350 | Medicare-compliant testing |
| Nox T3s | Professional-grade | 6 (RIP, nasal pressure, SpO2) | 88-92% | $300-$500 | High-pressure patients, clinical accuracy |
| Lofta Home Sleep Test | Full service kit | 4-5 channels | 85-88% | $189 all-inclusive | Complete service with doctor consult |
2025 Innovation Spotlight: ResMed launched the NightOwl device across the US in April 2025, featuring a disposable fingertip sensor that eliminates the need for nasal cannulas entirely. Early clinical data shows 87% concordance with polysomnography for AHI classification.

Home Sleep Test vs Sleep Lab: Which Do You Need?
While home sleep apnea tests work excellently for most patients with suspected OSA, certain situations require the comprehensive monitoring of in-lab polysomnography. Understanding when each test is appropriate ensures you get the right diagnosis.
| Feature | Home Sleep Test (HSAT) | In-Lab Polysomnography (PSG) |
|---|---|---|
| Location | Your own bedroom | Sleep laboratory facility |
| Channels Monitored | 3-7 (respiratory-focused) | 16+ (including brain waves) |
| Sleep Staging | Limited or estimated | Full EEG-based staging |
| Can Diagnose | Obstructive sleep apnea | OSA, central apnea, narcolepsy, parasomnias, PLM |
| Technician Present | No | Yes, all night |
| Typical Cost | $150-$500 | $1,500-$3,500 |
| Insurance Coverage | Usually covered with referral | Usually covered with referral |
| Results Timeline | 2-5 business days | 5-14 business days |
When HSAT is Appropriate
- High pre-test probability of moderate-to-severe OSA (loud snoring, witnessed apneas, daytime sleepiness)
- No significant cardiopulmonary disease
- No suspected comorbid sleep disorders (narcolepsy, insomnia, REM behavior disorder)
- Ability to follow device instructions independently
When You Need In-Lab Polysomnography
- Suspected central sleep apnea or complex sleep apnea
- Significant heart failure, COPD, or neuromuscular disease
- Suspected narcolepsy, parasomnia, or periodic limb movement disorder
- Negative or inconclusive HSAT despite strong symptoms
- CPAP titration study needed for treatment planning
How to Use a Home Sleep Apnea Test: Step-by-Step Guide
Proper setup is crucial for obtaining accurate results from your home sleep test. While each device has specific instructions, these general steps apply to most HSAT systems:
Obtain Your Device
After receiving a prescription from your doctor, get your HSAT device from a sleep clinic, medical supplier, or direct-to-consumer service. Ensure the device arrives with complete instructions and all components.
Prepare the Environment
Create a normal sleep environment. Sleep in your usual bed, at your regular time. Avoid alcohol for 24 hours before testing, and skip naps on testing day to ensure adequate sleep drive.
Apply Sensors Correctly
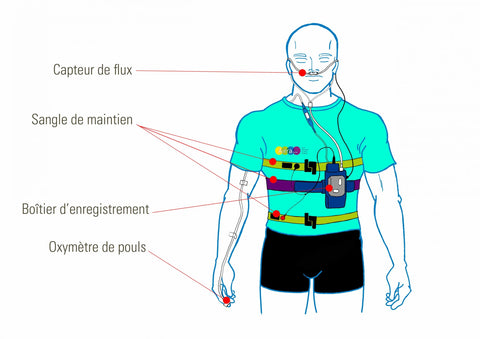
For most devices: attach the chest strap snugly, place the nasal cannula properly, and secure the finger pulse oximeter. The main recording unit should be positioned according to manufacturer instructions.
Activate and Sleep
Start the recording and try to sleep as normally as possible. Most devices require a minimum of 4-6 hours of usable data. If sensors become dislodged during the night, reattach them and continue sleeping.
Tips for Accurate Results
Maintain Your Routine - Go to bed and wake up at your normal times. The test should capture your typical sleep, not an artificially modified pattern.
Secure All Sensors - Use medical tape if needed to prevent sensors from shifting. Loose connections cause data gaps that may invalidate results.
Document Any Issues - Note if you woke frequently, had trouble falling asleep, or experienced sensor problems. This context helps interpret results.
Allow Extra Time - Plan for at least 7-8 hours in bed to ensure minimum data requirements are met, even if you sleep poorly.
Understanding Your Home Sleep Test Results
After your test, a board-certified sleep physician will analyze the data and provide a detailed report. Here are the key metrics you'll encounter:
The Apnea-Hypopnea Index (AHI)
The AHI is the primary diagnostic metric, representing the average number of apneas (complete breathing cessations) plus hypopneas (partial reductions) per hour of recording time.
| AHI Score | Classification | Clinical Significance | Typical Treatment Approach |
|---|---|---|---|
| <5 | Normal | No significant sleep apnea | Lifestyle modifications if symptomatic |
| 5-14 | Mild OSA | May contribute to snoring, mild fatigue | Positional therapy, oral appliances, nasal stents |
| 15-29 | Moderate OSA | Significant health impact, treatment recommended | CPAP, oral appliances, or combination therapy |
| 30+ | Severe OSA | Major cardiovascular and cognitive risks | CPAP as first-line, possibly with adjunctive therapies |
Other Important Metrics
Oxygen Desaturation Index (ODI)
Number of times per hour oxygen drops 3-4% or more. High ODI indicates significant oxygen deprivation during sleep, even if AHI appears lower.
Lowest SpO2
Your minimum oxygen saturation during the study. Values below 88% indicate severe desaturation; below 80% is critically low and requires urgent treatment.
Time Below 90% SpO2
Cumulative minutes spent with dangerously low oxygen. Extended hypoxia increases risk of cardiovascular complications and cognitive impairment.
Positional Data
Shows if apnea events cluster in certain sleep positions. Positional OSA (events primarily on back) may respond to simpler interventions.
Important: Home sleep tests may underestimate AHI compared to in-lab polysomnography because they calculate events per hour of recording time, not per hour of actual sleep. If your HSAT is negative but symptoms persist, discuss repeat testing or in-lab PSG with your doctor.
Home Sleep Test Cost and Insurance Coverage
Understanding the cost of home sleep testing helps you make informed decisions. Here's what to expect in 2026:
| Scenario | HSAT Cost | PSG Cost (Comparison) |
|---|---|---|
| Self-Pay (No Insurance) | $150-$500 | $1,500-$3,500 |
| With Insurance (After Deductible) | $0-$150 copay | $100-$500 copay |
| Medicare Coverage | 20% coinsurance (Part B) | 20% coinsurance (Part B) |
| HSA/FSA Eligible | Yes | Yes |
Medicare and Medicaid Coverage
Medicare Part B covers home sleep testing when ordered by a physician for suspected obstructive sleep apnea. The relevant CPT codes are:
- 95806: Sleep study, unattended, simultaneous recording (Type 3 HSAT)
- 95800: Sleep study, unattended with actigraphy
- G0398-G0400: Home sleep test services under Medicare guidelines
Most private insurers cover HSAT as the first-line diagnostic test for uncomplicated suspected OSA, often preferring it over in-lab studies due to lower cost.
Find Testing Services Near YouNext Steps After Your Home Sleep Test
Receiving a sleep apnea diagnosis is just the beginning of your journey to better sleep. Here's what typically happens next:
Review Results with Your Doctor
Schedule a follow-up appointment to discuss your HSAT results in detail. Your physician will explain your AHI, oxygen data, and recommend appropriate treatment based on severity and your specific circumstances.
Explore Treatment Options
Treatment depends on severity. Options include CPAP therapy, oral appliances, positional therapy, surgery, or innovative alternatives like the Back2Sleep nasal orthosis for mild-moderate cases.
Begin Treatment
If CPAP is prescribed, you may need a titration study to determine optimal pressure. Non-CPAP treatments can often begin immediately, providing faster relief from symptoms.
Follow-Up and Monitoring
Regular follow-up ensures treatment effectiveness. Many patients benefit from retesting after 3-6 months to verify improvement in AHI and oxygen levels.
Treatment Options by Severity
Mild OSA (AHI 5-14)
Lifestyle changes, positional therapy, nasal dilators like Back2Sleep, or oral appliances often provide excellent results without CPAP.
Moderate OSA (AHI 15-29)
CPAP is typically recommended but oral appliances and combination therapies are effective alternatives for CPAP-intolerant patients.
Severe OSA (AHI 30+)
CPAP is the gold standard. Surgical options or hypoglossal nerve stimulation may be considered for CPAP failure cases.
Positional OSA
When apnea occurs primarily in supine position, positional therapy devices or tennis ball technique may suffice as standalone treatment.
The Back2Sleep Alternative for Mild-Moderate Sleep Apnea
Studies show that 50% of CPAP users abandon therapy within the first year due to discomfort, claustrophobia, or lifestyle constraints. The Back2Sleep intranasal orthosis offers an effective alternative for patients with mild-to-moderate OSA who struggle with traditional CPAP.

How Back2Sleep Works
The Back2Sleep nasal stent is a soft, flexible intranasal device that maintains airway patency by gently keeping nasal passages open throughout the night. Unlike external nasal strips, it provides internal support where obstruction typically occurs.
Immediate Relief - Works from the first night without any adaptation period or pressure adjustments.
No Machine Required - Completely silent, no electricity needed, perfect for travel and camping.
Partner-Friendly - Virtually invisible and soundless, unlike the noise and hoses of CPAP machines.
Cost-Effective - Lower initial investment and no ongoing supply costs compared to CPAP equipment.
Frequently Asked Questions About Home Sleep Apnea Testing
Home sleep tests achieve 68-91% accuracy for diagnosing moderate-to-severe obstructive sleep apnea when used in appropriate patient populations. The WatchPAT device shows the highest concordance with polysomnography at approximately 89-91%. However, HSAT may miss mild sleep apnea in 30-40% of cases due to the way it calculates AHI (using recording time rather than actual sleep time). If your home test is negative but you still experience symptoms like loud snoring, witnessed apneas, or excessive daytime sleepiness, discuss in-lab polysomnography with your doctor.
Self-pay costs for home sleep testing typically range from $150 to $500, depending on the device and service provider. All-inclusive services like Lofta ($189) include the device, physician interpretation, and follow-up consultation. With insurance, out-of-pocket costs are usually $0-$150 after deductible. Medicare Part B covers HSAT with 20% coinsurance. In comparison, in-lab polysomnography costs $1,500-$3,500 self-pay or $100-$500 with insurance.
Yes, most insurance plans cover home sleep testing when prescribed by a physician for suspected obstructive sleep apnea. Medicare Part B covers HSAT under CPT codes 95806, 95800, and G0398-G0400. Many insurers actually prefer HSAT over in-lab studies as a cost-saving measure. Check with your specific plan for coverage details, pre-authorization requirements, and in-network providers.
The WatchPAT ONE and ResMed NightOwl are currently considered the most accurate consumer-accessible devices. WatchPAT offers the most comprehensive data including sleep staging, while NightOwl (launched April 2025) provides the simplest setup with a single fingertip sensor. For Medicare-compliant testing, the Alice NightOne and Nox T3s are widely used by sleep clinics. The "best" device depends on your specific needs, physician preference, and insurance coverage.
A home sleep test can provide data sufficient to diagnose obstructive sleep apnea, but the final diagnosis must come from a qualified healthcare provider, typically a board-certified sleep physician. The device collects the data; the doctor interprets it in the context of your symptoms, medical history, and physical examination. Self-interpretation of results is not recommended, as nuanced factors affect diagnosis and treatment decisions.
Home sleep tests measure breathing airflow (via nasal pressure sensors), oxygen saturation (via pulse oximetry), heart rate, and often body position and movement. Advanced devices like WatchPAT also estimate sleep stages using peripheral arterial tone (PAT) technology. HSAT does not measure brain waves (EEG), eye movements, or muscle activity like in-lab polysomnography, which is why it cannot diagnose conditions like narcolepsy or REM sleep behavior disorder.
The actual test requires one night of sleep, typically 6-8 hours in bed. Setup takes 10-20 minutes depending on the device. After returning the equipment, results are usually available within 2-5 business days. Some services offer same-week follow-up consultations. The entire process from device delivery to diagnosis can take as little as one week, compared to 4-8 weeks for scheduling an in-lab sleep study.
Take the First Step Toward Better Sleep
Whether you're preparing for a home sleep test or looking for treatment after diagnosis, Back2Sleep provides effective, comfortable relief from snoring and mild-moderate sleep apnea.
Get Your Back2Sleep Starter KitRelated Articles: Polysomnography Guide | Sleep Polygraphy Explained | Understanding Sleep Apnea | Contact Our Sleep Experts








